Dimension: Maternity Services
The aim of publishing metrics from each maternity unit in the RCSI Hospital Group is to enable patients, relatives and the general public to view activity in each of the three maternity units in the Group, (Cavan General Hospital, Drogheda Hospital and the Rotunda Hospital).
These metrics are comprised of a range of clinical activities, major obstetric events, modes of delivery and rates of attendance at clinical training.
When viewing these metrics, it is important to note that tertiary and referral maternity centres will care for a higher complexity of patients (mothers and babies). Therefore, rates of clinical activity and outcomes will be higher and comparisons should not be drawn with units that do not look after complex cases. In addition these figures are not formatted in a way to support comparison with other hospitals or aggregation with other data.
Demonstrates the volume of clinical activity in each organisation and information is reported on the total number of mothers delivered, the total numbers of births, the number of multiple pregnancies, and transfers in and out to hospitals.
Measurement methodology and data sources:
Local extracts submitted monthly and extrapolated for analysis and publication.
Target
These figures are not formatted in a way to support comparison with other hospitals or aggregation with other data.
Performance
(n) = number
Total mothers delivered >500g: Total number of women delivering a baby weighing 500g or more. The infant weight of 500g is an internationally recognised weight measurement for counting numbers of mothers delivered.
Multiple pregnancies: Number of mothers delivering more than one baby from a single pregnancy. This is a count of mothers, not numbers of babies delivered.
Total births >500g: Total number of babies born, including live births and stillbirths, weighing 500g or more. The weight of 500g is an internationally recognised weight measurement for counting numbers of babies born.
In-utero transfers admitted: Number of pregnant women admitted to a maternity hospital from another hospital prior to delivery for reasons in the fetal/maternal interest.
In-utero transfers sent out: Number of pregnant women transferred from a maternity hospital to another hospital prior to delivery for reasons in the fetal/maternal interest.
HOME BIRTHS
Introduction
Currently in Ireland there is a National Domiciliary Midwifery service available to eligible expectant mothers who wish to avail of a home birth service under the care of a self employed community midwife (SECM). This service is provided by the SECM on behalf of the HSE1.
Rationale for measurement
Research shows that a planned home birth is an acceptable and safe alternative to a planned hospital birth for some pregnant women. The expectant mother, in consultation with her midwife and other Medical advisors of her choice, can decide whether home birth is a safe option for her and her baby1.
Target
These figures are not formatted in a way to support comparison with other hospitals or aggregation with other data.
Performance
References:
1 HSE (2022) National Home Birth Services
MIDWIFERY LED UNITS (MLUS)
Introduction
Midwife-led maternity care is shown to be safe for women with low-risk during pregnancy. In Ireland, two midwife-led units (MLUs) were introduced in 2004. These are based in the RCSI HG in Drogheda and Cavan Hospitals. In the MLU a small team of midwives provide care for women throughout their pregnancy, during labour and in the postnatal period.
Rationale for measurement
A number of studies have found that midwife-led care leads to a number of positive outcomes with no adverse effects for mothers and their babies. In fact, midwifery care for women at low-risk for complications during pregnancy is associated with various benefits, such as increased rates of maternal satisfaction and a decrease in unnecessary medical intervention1-3.
Target
These figures are not formatted in a way to support comparison with other hospitals or aggregation with other data.
Performance
References:
1 Chapman, S. (2016), Midwife-led continuity models versus other models of care: review and reflections, https://www.evidentlycochrane.net {Accessed 13 June 2023}
2 Devane D, Begley C, Clarke M, Walsh D, Sandall J, Ryan P, Revill P, Normand C (2010). Socio-economic value of the midwife: A systematic review, meta-analysis, meta-synthesis and economic analysis of midwife-led models of care. London: RCM.
3 Cummins, A. Coddington, R. Fox, D. Symon, A. (2020) Exploring the qualities of midwifery-led continuity of care in Australia (MiLCCA) using the quality maternal and newborn care framework. Women and Birth, Volume 33, Issue 2.
PERINATAL MORTALITY RATE (ADJUSTED)
Definition
The Adjusted Perinatal Mortality Rate is defined as Stillbirth and early neonatal death > 2500 grams excluding lethal congenital defects/1000 deliveries.
Rationale for measurement
The perinatal mortality rate is recognised as an indicator of the quality and safety of antenatal and perinatal care.
Measurement methodology and data sources:
Local data extracts submitted monthly and extrapolated for analysis and publication.
Target
The figures beneath are not formatted in a way to support comparison with other hospitals or aggregation with other data. Context is provided in the graph in section ‘Perinatal Deaths ≥2.5kg without a Congenital Anomaly (Perinatal Adjusted)’.
Performance
- August 2024 Perinatal Mortality Rate (Adjusted) for Cavan (9.6) was above the national rate of 0.83 (95% CI ±0.60-1.06, IMIS 2021). August 2024 Perinatal Mortality Rate (Adjusted) for Drogheda Hospital (0) was below the national rate of 0.83 (95% CI ±0.60-1.06, IMIS 2021). Q2-2024 Perinatal Mortality Rate (Adjusted) for Rotunda Hospital (0.93) was within the Confidence Interval of 95% ±0.60-1.06 (IMIS 2021).
PERINATAL DEATHS ≥2.5KG WITHOUT A CONGENITAL ANOMALY (PERINATAL ADJUSTED)
Rationale for measurement
Perinatal mortality Rate – Adjusted (PNMR-A) is defined as the number of perinatal deaths (stillbirths and early neonatal deaths) weighing 2.5kg or more without physiological or structural abnormalities that develop at or before birth and are present at the time of birth per 1,000 births. PNMR-Adjusted is an important indicator of the quality of care provided in Irish maternity services.
Measurement methodology and data sources:
Maternity Units in the Rotunda, Drogheda and Cavan Hospitals submit perinatal mortality data on a monthly basis to the RCSI HG, which in turn is made available to the National Women and Infants Health Programme Clinical Programme Irish Maternity Indicator System (IMIS). The IMIS report is published on an annual basis and allows scrutiny of individual hospital processes and outcomes for women and infants, while bench marking them against national performance.
Variations in PMR – Adjusted between maternity units could potentially be due to random chance or reflect differences in baseline characteristics of the childbearing population. For this reason, funnel plots are used to assess performance outcomes for individual maternity units in comparison to the overall average. The funnel plot is a scatter diagram of individual maternity unit mortality rates against the total number of births within that unit.
In the funnel graph below:-
- The national rate for PNMR-A is indicated by the solid straight green line for 2021 and by a dashed grey line for 2020
- The curved dashed lines (the 95% confidence interval for 2021) represent the limits within which 95% of units are expected to lie
- Solid diamond-shaped markers represent the RCSI HG maternity hospitals/units
- The width of the confidence interval is adjusted to allow for meaningful comparison between unit-specific rates and the national rate. The confidence interval is wider for smaller units reflecting the lack of precision in rates calculated based on small numbers. The confidence interval narrows for larger maternity units, giving the diagram a ‘funnel’ shape.
Performance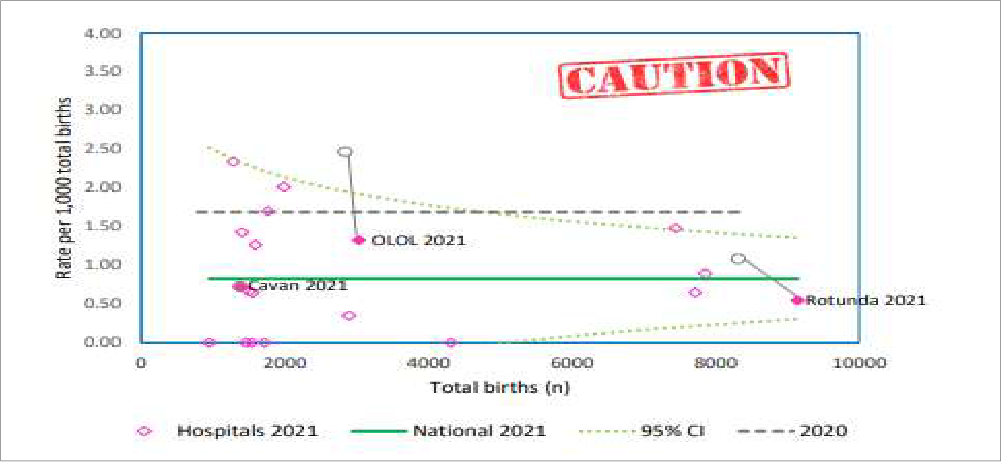
Note:
Maternity units include in their figures of perinatal deaths babies that are transferred in utero from other units and die in their hospital. Annual rates of perinatal deaths ≥2.5kg without a congenital anomaly should be interpreted with caution.
Drogheda, Cavan and Rotunda are all within the 95% confidence interval for 2021 (curved dashed lines).
NEONATAL ENCEPHALOPATHY (NE)
Rationale for measurement
Neonatal encephalopathy (NE) is a complex disease of a new-born infant and can be defined as clinical findings in three or more of the following domains: level of consciousness, spontaneous activity when awake or aroused, posture, tone, primitive reflexes, and autonomic system. NE can result from a wide variety of causes. Hypoxic Ischaemic Encephalopathy (HIE) is a subset of NE and is the most common cause of NE; however not all encephalopathies have a HIE.
Measurement methodology and data sources:
Maternity Units in the Rotunda, Drogheda and Cavan Hospitals submit perinatal mortality and morbidity data on a monthly basis to the RCSI HG, which in turn is made available to the National Women and Infants Health Programme Clinical Programme Irish Maternity Indicator System (IMIS). The IMIS report is published on an annual basis and allows scrutiny of individual hospital processes and outcomes for women and infants, while bench marking them against national performance.
Variations in Neonatal Encephalopathy (NE) rates between maternity units could potentially be due to random chance or reflect differences in baseline characteristics of the childbearing population. For this reason, funnel plots are used to assess performance outcomes for individual maternity units in comparison to the overall average. The funnel plot is a scatter diagram of individual maternity unit mortality rates against the total number of births within that unit.
In the funnel graph below:-
- The national rate NE is indicated by the solid straight green line for 2021 and by a dashed grey line for 2020
- The curved dashed lines (the 95% confidence interval for 2021) represent the limits within which 95% of units are expected to lie
- Solid diamond-shaped markers represent the RCSI HG maternity hospitals/units
- The width of the confidence interval is adjusted to allow for meaningful comparison between unit-specific rates and the national rate. The confidence interval is wider for smaller units reflecting the lack of precision in rates calculated based on small numbers. The confidence interval narrows for larger maternity units, giving the diagram a ‘funnel’ shape.
Performance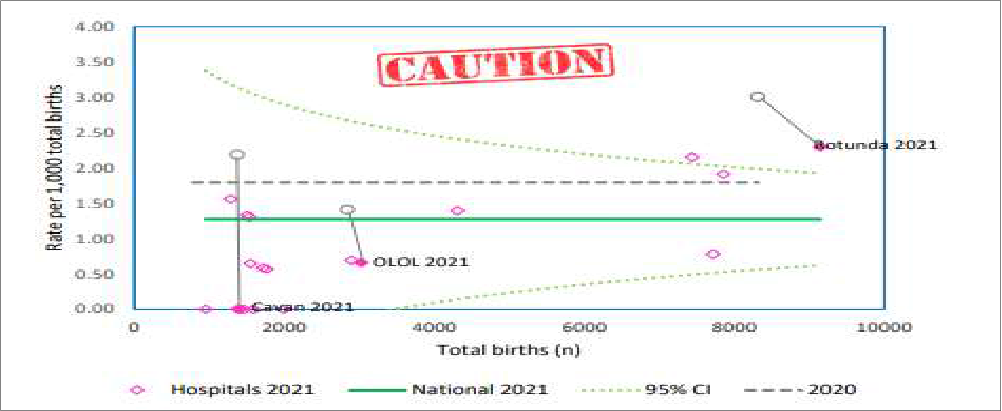
Description: All infants with ≥35 weeks’ gestation who, during the first week of life, have either seizures alone and/or signs of neonatal encephalopathy. Caution is advised when dealing with small values
Drogheda and Cavan are within the 95% confidence interval for 2021 (curved dashed lines)
Rotunda is outside the 95% confidence interval for 2021 (curved dashed line)
BREASTFEEDING RATES
Introduction
Breastfeeding, also called nursing, is the process of feeding human breast milk to a child, either directly from the breast or by expressing (pumping out) the milk from the breast and bottle-feeding it to the infant. The World Health Organization (WHO) recommends that breastfeeding begin within the first hour of a baby’s life and continue as often and as much as the baby wants. (1)
Rationale for measurement
Breastfeeding has many health benefits for both the mother and infant. Breast milk contains all the nutrients an infant needs in the first six months of life. Breastfeeding protects against diarrhoea and common childhood illnesses such as pneumonia and may also have longer-term health benefits for the mother and child, such as reducing the risk of overweight and obesity in childhood and adolescence. WHO recommends that infants should be exclusively breastfed for the first six months of life to achieve optimal growth, development and health.
IMIS Rates
Measurement methodology and data sources
Maternity Units in the Rotunda, Drogheda and Cavan Hospitals submit perinatal data on a monthly basis to the RCSI Hospital Group, which in turn is made available to the National Women and Infants Health Programme Clinical Programme Irish Maternity Indicator System (IMIS). The IMIS report is published on an annual basis and allows scrutiny of individual hospital processes and outcomes for women and infants, while bench marking them against national performance.
Variations in breast feeding rate between maternity units could potentially be due to random chance or reflect differences in baseline characteristics of the childbearing population. For this reason, funnel plots are used to assess breast feeding rates for individual maternity units in comparison to the overall average. The funnel plot is a scatter diagram of individual maternity unit breast feeding rates against the total number of births within that unit.
In the funnel graph below:
- the national rate for breast feeding in 2021 is indicated by the solid straight green line
- the curved dashed lines (the 95% confidence interval for 2021) represent the limits within which 95% of units are expected to lie.
- the width of the confidence interval is adjusted to allow for meaningful comparison between unit-specific rates and the national rate. The confidence interval is wider for smaller units reflecting the lack of precision in rates calculated based on small numbers. The confidence interval narrows for larger maternity units, giving the diagram a ‘funnel’ shape.
- Cavan Hospital has missing/incomplete data in 2021. Cavan Hospital is represented by an unfilled dot (2020 data)
Reference
- American Academy of Pediatrics Section on Breastfeeding. (March 2012). “Breastfeeding and the use of human milk”. Pediatrics. 129(3): e827-41. doi:1542/peds.2011-3552. PMID 22371471
Performance
Breastfeeding initiated
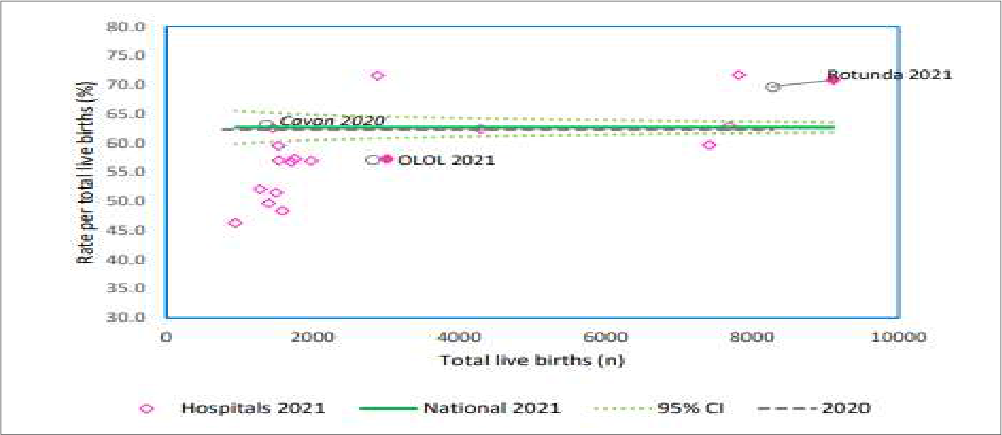
- nationally, in 2021, 62.7% of woman initiated breastfeeding at their baby’s first feed
- Rotunda Hospital had a rate of 70.8% which is above the national average
- Drogheda had a rate of 58.3% which is below the national average
- Cavan Hospital has missing/incomplete data in 2021. Cavan Hospital is represented by an unfilled dot (2020 data)
Breastfeeding (BF) exclusively on discharge
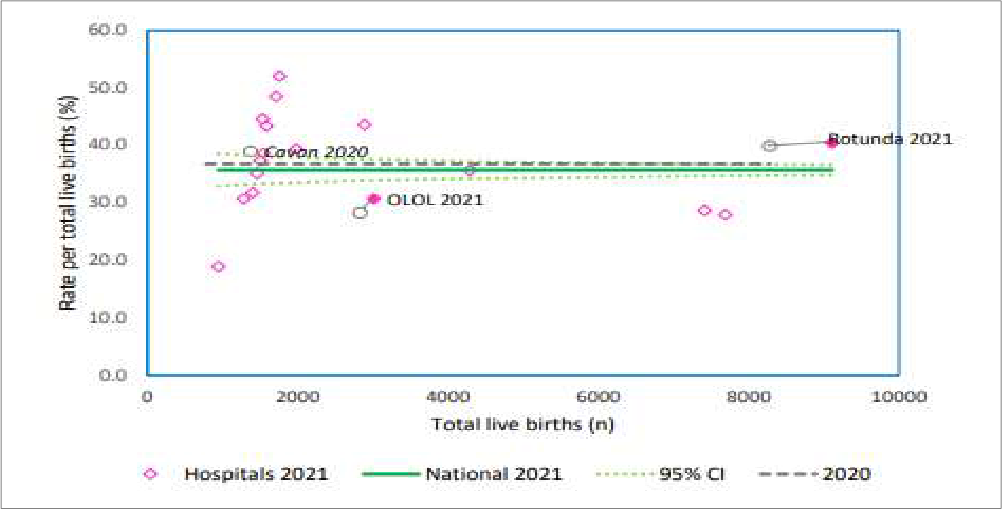
- nationally, in 2021, 35.6% of women were breast-feeding exclusively on discharge
- within the RCSI Hospital Group, Rotunda had a rate of 40.4% which is above the national average
- Drogheda had a rate of 30.6% which was below the national average
- Cavan Hospital has missing/incomplete data in 2021. Cavan Hospital is represented by an unfilled dot (2020 data)
Breastfeeding (BF) non-exclusively on discharge
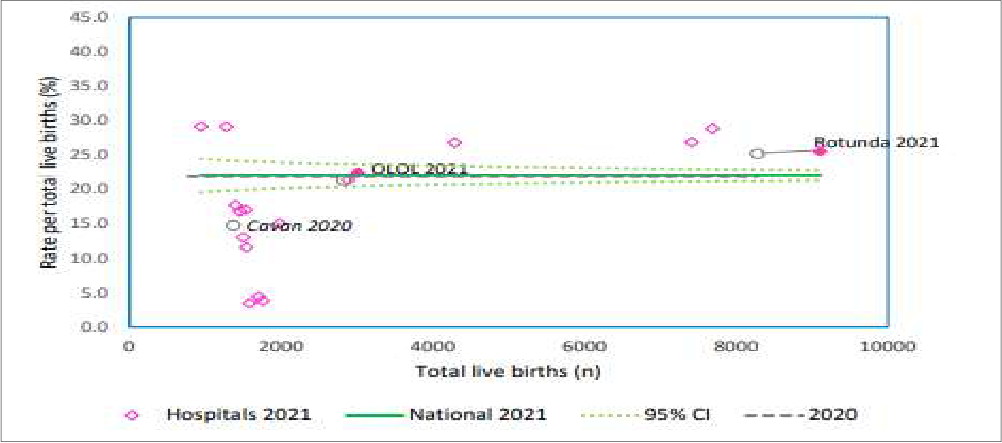
- nationally, in 2021, 22% of women were breast-feeding exclusively on discharge
- within the RCSI Hospital Group, both the Rotunda (25.5%) and Drogheda (22.4%) are both above the national average for breast-feeding non-exclusively on discharge.
- Cavan Hospital has missing/incomplete data in 2021. Cavan Hospital is represented by an unfilled dot (2020 data)
RCSI Hospital Breast Feeding Rates
Measurement methodology and data sources
Breastfeeding initiated: Numbers of babies breastfed at first feed following birth, i.e., direct from the breast or expressed. Rate is calculated per total live births. Nationally, in 2021, 62.7% of woman initiated breastfeeding at their baby’s first feed (IMIS 2021).
Breastfeeding (BF) exclusively on discharge: Numbers of babies who receive only breast milk without any additional food or drink, not even water, prior to discharge. Rate is calculated per total live births. Nationally, in 2021, 35.6% of woman were breast-feeding exclusively on discharge (IMIS 2021).
Breastfeeding (BF) non-exclusively on discharge: Number of babies who were breastfed and had other food or drink prior to discharge. Rate is calculated per total live births. Nationally, in 2020, 22% of woman were breast-feeding non-exclusively on discharge (IMIS 2021).
Maternity Units in the Rotunda, Drogheda and Cavan Hospitals submit perinatal data on a monthly basis to the RCSI Hospital Group. This data is also made available to the National Women and Infants Health Programme Clinical Programme Irish Maternity Indicator System (IMIS).
Performance
- in Q2 2024 Drogheda Hospital is below the national rate for breast feeding initiated and breast feeding exclusively (on discharge)
- in Q2 2024 Cavan Hospital is above the national rate for breast feeding initiated and breast feeding exclusively (on discharge)
- in Q2 2024 the Rotunda Hospital is above the national rate for breast feeding initiated and below the national rate for breast feeding exclusively (on discharge)
These are rare but potentially catastrophic events, which when they occur in obstetric patients can impact on the safety of both mother and baby. The RCSI Hospital Group reports the total combined rate (per 1,000 total mothers delivered) of the following major obstetric events,
- Eclampsia is a condition in which one or more convulsions occur in a pregnant woman suffering from high blood pressure, often followed by coma and posing a threat to the health of mother and baby.
- Uterine rupture is a rare but potentially catastrophic event in which the uterus tears open along the scar line from a previous Caesarian-section or major uterine surgery. Hospital incidence of uterine rupture is rare. The main risk factors for uterine rupture are previous caesarean section or induction of labour (using prostaglandins).
- Peripartum hysterectomy is a hysterectomy which is usually performed following a caesarean section, but also includes hysterectomies performed during pregnancy and/or within seven completed days after delivery. Peripartum hysterectomy is rare and usually only performed in emergency situations, but it is a life-saving procedure in cases of severe haemorrhage.
- Pulmonary embolism (PE) is a blockage of the lung’s main artery or one of its branches by a substance that travels from elsewhere in the body through the bloodstream.
Measurement methodology and data sources:
Local data extracts submitted monthly and extrapolated retrospectively for analysis and publication.
Numerator: Number of events
Denominator: per 1,000 total mothers delivered
Target
These figures are not formatted in a way to support comparison with other hospitals or aggregation with other data.
Performance
RATE OF OPERATIVE VAGINAL DELIVERY (OVD)
Rationale for measurement
Operative Vaginal Delivery (OVD) or Instrumental delivery: Percentage of ‘Mothers delivered ≥500g’ who require instrumental assistance during delivery. Instrumental assistance includes forceps delivery and vacuum extraction, excluding failed forceps and failed vacuum extraction. Also includes assisted breech delivery with forceps to after coming head and breech extraction with forceps to after-coming head.
Most women aim for spontaneous vaginal delivery. An instrumental delivery may be performed in situations where imminent delivery of the infant is considered to be the safest option for both mother and baby.
Measurement methodology and data sources:
Local data extracts submitted monthly and extrapolated for analysis and publication.
Numerator: Rate of instrumental deliveries (%)
Denominator: per 1,000 total mothers delivered
National Performance
National Operative Vaginal Delivery rate = 13.5% (95% Confidence Intervals 13.3-13.8%), Irish Maternity Indicator System (IMIS) Report 2021.
Performance
Cavan Hospital
- Cavan (August data) is below the 2021 national rate for operative vaginal delivery per total mothers delivered
Drogheda Hospital
- Drogheda (August data) is below the 2021 national rate for operative vaginal delivery per total mothers delivered
Rotunda Hospital
- Rotunda Hospital (August data) is above the 2021 national rate for operative vaginal delivery per total mothers delivered
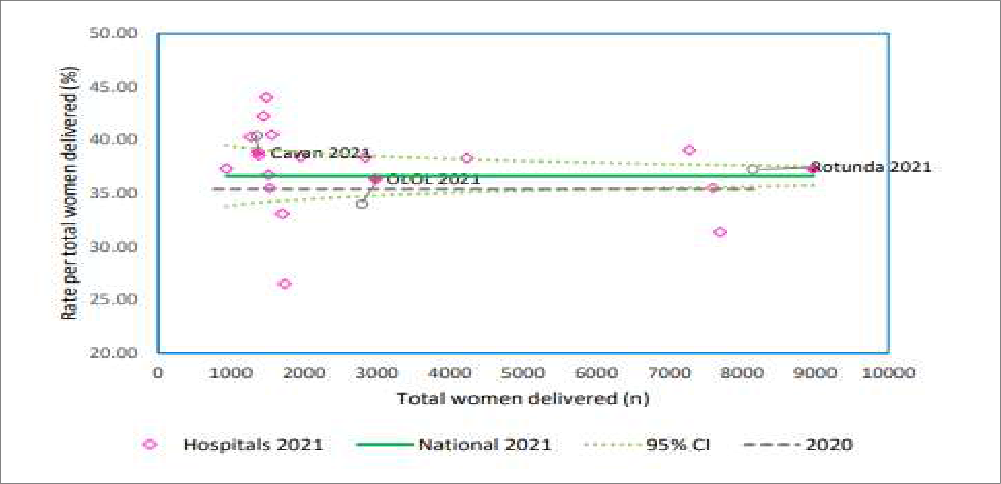
RATE OF INDUCTION OF LABOUR
National Performance
National rate for induction of labour = 35.1% (95% Confidence Intervals of 34.7-35.4%), Irish Maternity Indicator System (IMIS) Report 2021
Performance
Cavan Hospital
- Cavan (August data) is above the 2021 national rate for induction of labour per total mothers delivered
Drogheda Hospital
- Drogheda (August data) is above the 2021 national rate for induction of labour per total mothers delivered
Rotunda Hospital
- Rotunda Hospital (August data) is above the 2021 national rate for induction of labour per total mothers delivered
RATE OF CAESAREAN SECTION
Rationale for measurement
Caesarean delivery, also known as a C-section, is a surgical procedure used to deliver a baby through incisions in the mother’s abdomen and uterus. When medically justified, a Caesarean Section can reduce problems/complications for mother and baby (mortality and morbidity). Recovery from a C-section takes longer than does recovery from a vaginal birth. Like other types of major surgery, C-sections also carry risks. It is acknowledged that Caesarean rates are on the rise in many developed countries. Ireland’s National Maternity Strategy (2016) identifies a number of possible reasons for this – including “reductions in the risk of Caesarean delivery, increasing litigation, increases in first births among older women and the rise in multiple births resulting from assisted reproduction.”
Measurement methodology and data sources:
Monthly Performance
Local data extracts submitted monthly and extrapolated for analysis and publication
National Performance
National rate for Caesarean Section = 36.6% (95% Confidence Intervals 36.2-37.0%), Irish Maternity Indicator System (IMIS) Report, 2021
Performance
Cavan General Hospital
- Cavan (August data) is above the 2021 national rate for Caesarean Section per total mothers delivered
Drogheda Hospital
- Drogheda (August data) is above the 2021 national rate for Caesarean Section per total mothers delivered
Rotunda Hospital
- Rotunda Hospital (August data) is above the 2021 national rate for Caesarean Section per total mothers delivered
CAESAREAN SECTION RATE (IMIS)
Measurement methodology and data sources
Irish Maternity Indicator System (IMIS)
The C-section rate is comprised of the numbers of women in each maternity unit who give birth by C-section. This data is divided into first time mothers (nulliparous women), mothers who have given birth previously (multiparous women) and the total C-section rate.
Maternity Units in the Rotunda, Drogheda and Cavan Hospitals submit data on C-section numbers on a monthly basis to the RCSI Hospital Group, which in turn is made available to the National Women and Infants Health Programme and the Irish Maternity Indicator System (IMIS). The IMIS report1 is published on an annual basis and allows scrutiny of individual hospital processes and outcomes for women and infants, while benchmarking them against national performance.
Variations in C-section Rates adjusted between maternity units could potentially be due to random chance or reflect differences in baseline characteristics of the childbearing population. For this reason, funnel plots are used to assess performance outcomes for individual maternity units in comparison to the overall average. The funnel plot is a scatter diagram of individual maternity unit C-section rates.
In the funnel graphs below: The national rate for C-section Rate is indicated by the solid straight green line for 2021 and by a dashed grey line for 2020 – The curved dashed lines (the 95% confidence interval for 2021) represent the limits within which 95% of units are expected to lie. The width of the confidence interval is adjusted to allow for meaningful comparison between unit-specific rates and the national rate. The confidence interval is wider for smaller units reflecting the lack of precision in rates calculated based on small numbers. The confidence interval narrows for larger maternity units, giving the diagram a ‘funnel’ shape.
Performance
Total Caesarean section
- Cavan, Drogheda and the Rotunda Hospitals are within the 95% confidence intervals for the total numbers of women giving birth by C-section
Caesarean section – nulliparas women 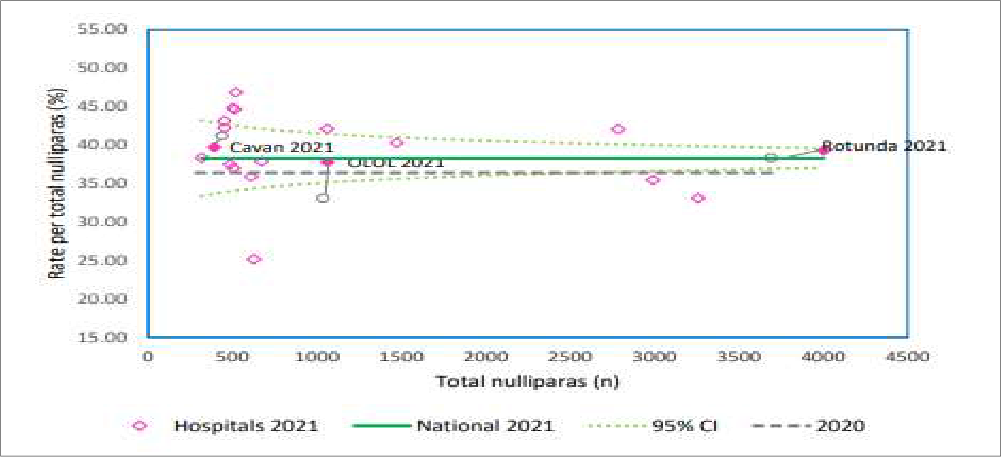
- Cavan, Drogheda and the Rotunda Hospitals are within the 95% confidence intervals for nulliparas women giving birth by C-section
Caesarean section – multiparas women 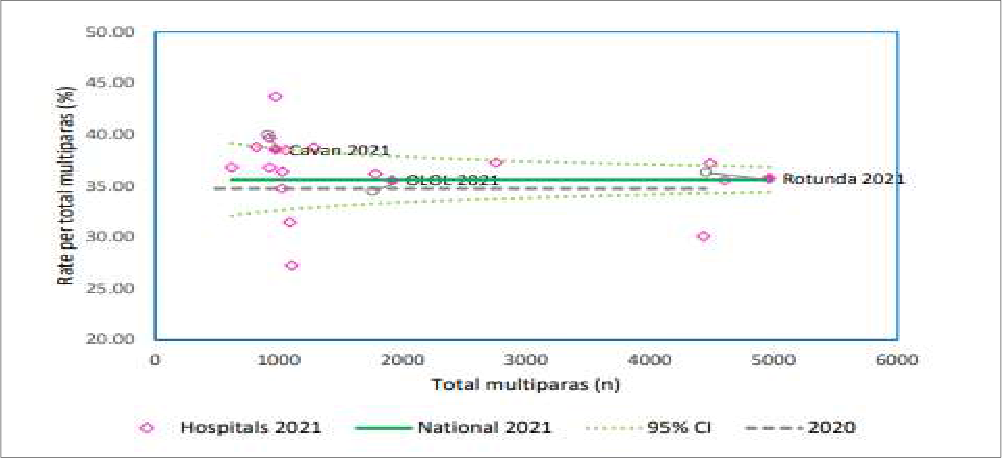
- Cavan, Drogheda and the Rotunda Hospitals are within the 95% confidence intervals for multiparas women giving birth by C-section
References
1 IMIS Report, 2021
Introduction
The fetal anomaly scan is a detailed scan carried out in pregnant women at about 20 weeks’ gestation (mid pregnancy) to check if the baby is developing normally. Prenatal scanning is of great importance as it contributes to appropriate management of the baby both during and after the pregnancy. Fetal anomaly scanning is very accurate but unfortunately it cannot identify all birth defects.
Rationale for measurement
Prior to November 2017, Fetal Anomaly Scanning for women in the North East was available only if they were referred to the Rotunda Hospital or if they chose to access this service privately
A fetal anomaly scanning service is now available in Louth Hospitals and Cavan/Monaghan Hospitals. The RCSI Hospital Group monitors the numbers of women availing of this service across the three maternity units of the RCSI Hospital Group, Cavan, Monaghan, Louth Hospitals and the Rotunda Hospital.
Measurement methodology and data sources
(1) number of women booked and
(2) number of fetal anomaly scans performed – Local Hospital data extrapolated for analysis and publication
Performance
- capacity available for all bookings. Option to attend facilities external for scan is available to all women
