Dimension: Patient Care and Treatment
Rationale for measurement
A number of measures are also outlined which reflect the outcomes of care for patients undergoing emergency hip surgery. These reflect the standards outlined in the Irish Hip Fracture Database National Office of Clinical Audit:
- Percentage admitted within 4 hours to orthopaedic ward: All patients with hip fracture should be admitted to an acute orthopaedic ward within 4 hours of presentation or brought to the theatre from the ED within 4 hours
- Percentage who had surgery within 48 hours and during working hours: All patients with hip fracture who are medically fit should have surgery within 48 hours of admission and during normal working hours (Mon-Sun 8:00-17:59)
- Percentage of patients who developed a new pressure ulcer: All patients with hip fracture should be assessed and cared for with a view to minimising their risk of developing a pressure ulcer
- Percentage of patients seen by a Geriatrician during acute admission: All patients presenting with a fragility fracture should be managed on an orthopaedic ward with routine access to acute orthogeriatric medical support from the time of admission
- Percentage of patients who received a bone health assessment: All patients presenting with fragility fracture should be assessed to determine their need for therapy to prevent future osteoporotic fractures
- Percentage of patients who received specialist falls assessment: All patients presenting with a fragility fracture following a fall should be offered multidisciplinary assessment and intervention to prevent future falls
- Percentage of patients mobilised by physiotherapist: All patients with hip fracture surgery should be mobilised by a physiotherapist on the day of, or the day after, surgery
Measurement methodology and data sources
- Local Hospital HIPE data extrapolated for analysis, supplied one quarter in arrears.
Performance
- National Performance IHFD Data Quarter 2 2023 is published data by NOCA. National Performance for Quarters 3 and 4 2023 unavailable at time of report publication
- RCSI Hospital Group Performance Local Hospital IHFD Data Quarter 4 2023
- NOCA data contains all cases in relation to delays to theatre. NOCA data excludes patients <60 yrs of age
- note1 % of patients who had surgery within 48hrs and during working hours includes those medically unfit in first 48hrs
Falls particularly in the elderly can lead to an increased time spent in Hospital and in significant health decline. As well as physical injuries suffered, the psychological and social consequences of falling can have a huge impact. Recurrent falls in the elderly can result in long term care, consequently falls prevention is a key area for hospitals. Serious falls that have caused patient death or disability while being cared for in a healthcare facility are defined as serious reportable events (SRE) in Irish Hospitals. While all falls do not result in injury, they can cause distress and anxiety to patients and their families. All Hospitals in the RCSI Group are committed to preventing patient falls where possible, and where not possible to minimising their incidence and impact.
Measurement methodology and data sources
- Number of patient falls associated with Patient death or disability whilst being cared for in a health service facility per 10,000 hospital bed days
- Number of patient falls whilst being cared for in a health service facility per 10,000 hospital bed days
- Local data extrapolated from Hospital Performance Metrics
Target
- No patient falls associated with mortality or morbidity whilst being cared for in a health service facility
Performance
- the rate of 2.0 reported for February 2024 is higher than the rate of 0.4 reported for February 2023
- number of serious falls reported for RCSI HG YTD 2024 (n=17) vs YTD 2023 (n=7) demonstrating a 143% increase
- the rate of Serious Falls in Beaumont Hospital has increased in February 2024
- the rate of Serious Falls in Connolly Hospital has increased in February 2024
- the rate of Serious Falls in Cavan & Monaghan Hospitals has increased in February 2024
- the rate of Serious Falls in Drogheda & Louth Hospitals has decreased in February 2024
- RCSI Acute Hospitals reported a rate of 53.4 patient falls per 10,000 BDU (n=3,219) in Quarter 1-4 2023
- national values not available
Falls are one of the most frequently reported incidents for hospital inpatients. Falls particularly in the elderly can lead to an increased time spent in Hospital and in significant health decline. As well as physical injuries suffered, the psychological and social consequences of falling can have a huge impact. Consequently, prevention and injury management is a key priority in healthcare.
The Quality Care Metric indicators below check that patients at risk of falling are managed in accordance with local and national policies, procedures, protocols and guidelines (PPPGs).
- Falls risk assessment was recorded on admission/transfer if applicable
- If the patient is identified as at risk of falling, nursing interventions are in place to minimise the risk of falling
- The patient, if identified at risk of falling, has been offered information about falls
- If a patient has fallen, the relevant post falls documentation have been completed
Measurement methodology and data sources
Based on total bed capacity, samples of 25% of patient records are randomly selected per month from each ward/unit with a minimum of 5 data collections per month for each ward/unit. National Guideline for Nursing and Midwifery Quality Care Metrics Data Measurement in Acute Care (2018) outlines the essential criteria for measurement of data for recording of falls https://healthservice.hse.ie/filelibrary/onmsd/national-guideline-for-nursing-and-midwifery-quality-care-metrics-data-measurement-in-acute-care.pdf
Target
90% compliance of the key indicators identified. Quality Care Metrics KPI set is identified as ‘areas of good practice’ are demonstrated 90-100%; ‘areas requiring some improvement’ 80-89%; ‘areas requiring immediate attention and action plans’ 0-79%.
Performance – % Compliance – 2024
- RCSI Hospitals achieved target of 90% in February 2024
- national data not collected
Pressure ulcers, also called bedsores, are injuries to skin and underlying tissue resulting from prolonged pressure on the skin. Pressure ulcers most often develop on skin that covers bony areas such as heels, ankles, hips and tailbone. Hospitalised and immobile persons can be at risk of pressure ulcers. Pressure ulcers can cause pain, poor recovery and lead to serious infections. Pressure ulcers are graded Stage 1 to 4. At Stage 3, the ulcer is a deep wound with loss of skin and the damage may extend beyond the primary wound and below layers of healthy skin. At Stage 4, the ulcer shows large scale loss of tissue and may expose muscle, bone and tendon. Prevention of Grade 3 and Grade 4 bed ulcers are a marker of good care.
Measurement methodology and data sources
- Number of Stage 1 and 2 pressure ulcers per quarter
- Number of Stage 3 or 4 pressure ulcers per 10,000 hospital bed days
- Local data extrapolated from Hospital Performance Metrics
- National data extracted from the National Incident Management System (NIMS)
Definitions
- Stage 1: Intact skin with non–blanchable redness of a localised area usually over a bony prominence. Discolouration of the skin, warmth, oedema, hardness or pain may also be present. Darkly pigmented skin may not have visible blanching. The area may be painful, firm, soft, warmer or cooler as compared to adjacent skin
- Stage 2: Partial thickness skin loss of dermis presenting as a shallow ulcer with a red pink wound bed, without slough. May present as an intact or open/ ruptured serum filled blister filled with serous or sero-sanguineous fluid. Presents as a shiny or dry shallow ulcer without slough or bruising
- Stage 3: Full thickness tissue loss. Subcutaneous fat may be visible but bone, tendon or muscles are not exposed. Slough may be present but does not obscure the depth of tissue loss. This stage may include undermining and tunneling.
- Stage 4: Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present. This stage often includes undermining and tunneling. Exposed bone/muscle is visible or directly palpable.
Reference: European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory Panel. Prevention and treatment of pressure ulcers (2009)
- Local hospital data (no national comparator data available)
Target
- No grade 3/4 pressure ulcers (RCSI Hospital Group target)
Performance
RCSI Hospital Group
- the rate of 1.0 reported for February 2024 is higher than the rate of 0.6 reported for February 2023
- number of grade 3 and 4 pressure ulcers in RCSI HG YTD 2024 (n=19) vs YTD 2023 (n=16) demonstrating a 19% increase
- in February 2024 the rate of Pressure Ulcers in Beaumont Hospital is lower than the NIMS 2022 rate
- in February 2024 the rate of Pressure Ulcers in Connolly Hospital is lower than the NIMS 2022 rate
- in February 2024 the rate of Pressure Ulcers in Cavan & Monaghan Hospitals is lower than the NIMS 2022 rate
- in February 2024 the rate of Pressure Ulcers in Drogheda & Lough Hospitals is lower than the NIMS 2022 rate
- RCSI Acute Hospitals reported a rate of 7.6 pressure ulcers per 10,000 BDU (n=457) in Quarter 1-4 2023
Most pressure injuries can be avoided, providing individuals at risk are correctly identified and appropriate measures are put into place to combat risk (Pressure Ulcers: A Practical Guide to Review, HSE 2018).
The Quality Care Metric indicators below check that patients at risk of/with pressure Ulcers are managed in accordance with local and national policies, procedures, protocols and guidelines (PPPGs):
- A pressure ulcer risk assessment was recorded using a validated tool within 6 hours of admission or transfer
- If a patient is identified as at risk, daily skin inspections have been recorded
- The pressure ulcer risk was reassessed in response to any changes in the patient’s condition
- The pressure ulcer risk was reassessed weekly
- If a pressure ulcer is present, the category/stage has been recorded
- Reassessment and evaluation of the pressure ulcer have been completed
- The frequency of patient repositioning is recorded
- The use of pressure redistributing devices is recorded
Measurement methodology and data sources
Based on total bed capacity, samples of 25% of patient records are randomly selected per month from each ward/unit with a minimum of 5 data collections per month for each ward/unit.
Target
90% compliance of the key indicators identified. Quality Care Metrics KPI set is identified as ‘areas of good practice’ are demonstrated 90-100%; ‘areas requiring some improvement’ 80-89%; ‘areas requiring immediate attention and action plans’ 0-79%.
Performance – % Compliance – 2024
- RCSI Hospitals achieved target of 90% in February 2024 with the exception of Connolly Hospital
- national data not collected
Adequate food and hydration is fundamental to a person’s health and wellbeing. Nutrition and hydration in the acute hospital setting is an important element in the provision of safe quality care. Patients can be found to be malnourished when they are admitted to hospital and a patient’s nutritional status can deteriorate during a hospital stay. Therefore, malnutrition screening followed by an appropriate plan of care are seen as essential factors in recognising, managing and promoting improved nutritional and hydration status for patients in our care.
The Quality Care Metric indicators below check that Nutrition and Hydration nursing assessment, screening, and care planning are completed. This is in accordance with local policies, procedures, protocols and guidelines (PPPGs) and as documented in the Nutrition Screening and use of Oral Nutrition Support for Adults in the Acute Care Setting National Clinical Guideline No. 22 (DOH 2020) and the national Food Nutrition and Hydration Policy for Adult Patients in Acute Hospitals (HSE 2018).
- The patient’s risk of malnutrition has been screened on admission/transfer
- A plan of care has been developed based on the patient’s risk of malnutrition
- The patient’s risk of malnutrition has been re-screened
- The patient’s oral health status assessment has been completed
- The nursing care provided for the patient’s oral health has been documented
- Changes in the patient’s bowel pattern have been assessed, recorded and managed
Measurement methodology and data sources
Based on total bed capacity, samples of 25% of patient records are randomly selected per month from each ward/unit with a minimum of 5 data collections per month for each ward/unit
Target
90% compliance of the key indicators identified.
Performance – % Compliance – 2024
- Beaumont and Cavan & Monaghan Hospitals achieved target of 90% in February 2024
- Connolly and Drogheda Hospital did not achieve target of 90% in February 2024
- national data not collected
Readmissions rates can be influenced by a variety of factors, including the quality of inpatient and outpatient care, the effectiveness of the care transition and coordination, and the availability and use of effective disease management community based programmes. Whilst not all unplanned readmissions are avoidable, interventions during and after a hospitalisation can be effective in reducing rates (Government of Alberta – Alberta Health Service Plan 2014-2017).
Measurement Methodology and Data Sources
- local retrospective data extracted, extrapolated and published by HSE – BIU. Published one month in arrears.
Target
- Surgical readmission to same hospital within 30 days → ≤2% (NSP 2023)
- Medical readmission to same hospital within 30 days → ≤11.1% (NSP 2023)
Performance – Surgical
Beaumont Hospital
- Beaumont rate of 1.2%. National target achieved
Cavan Hospital
- Cavan rate of 3.8%. National target not achieved
Connolly Hospital
- Connolly rate of 1.8%. National target achieved
Drogheda Hospital
- Drogheda rate of 1.5%. National target achieved
RCSI Hospital Group
- RCSI Hospital Group rate of 1.7%. National target achieved
Performance – Medical
Beaumont Hospital
- Beaumont rate of 10.0%. National target achieved
Cavan Hospital
- Cavan rate of 7.2%. National target achieved
Connolly Hospital
- Connolly rate of 8.9%. National target achieved
Drogheda Hospital
- Drogheda rate of 9.0%. National target achieved
RCSI Hospital Group
- RCSI Hospital Group rate of 8.8%. National target achieved
Chronic obstructive pulmonary disease (COPD) is a disease of the lungs characterised by airflow obstruction. This airflow obstruction is usually progressive and only partially reversible. The disease is associated with increasing dyspnoea (breathlessness) and in more severe cases can be associated with exacerbations of the disease, which may require intervention either in primary care, attendance at the hospital or even admission to hospital. Patients with severe COPD may suffer frequent exacerbations of their disease requiring medical attendance, potential hospitalisation and severe disruption of their quality-of-life. (End to End COPD Model of Care, December 2019, National Clinical Programme for Respiratory).
Rationale for measurement
Ireland has the highest rate of hospitalisation for COPD of all Organisation for Economic Co-operation and Development (OECD) countries. In 2013 (the latest year for which OECD data are currently available), the age standardised hospitalisation rate in Ireland based on OECD age standardisation equated to an age-sex standardised rate of 395/100,000 is almost double the OECD average of 201 hospitalisations per 100,000 population. Early supported discharge from hospital can benefit patients as they receive treatment in their own home. In addition the risk of patients contracting a hospital acquired infection is reduced. The RCSI HG measures re-admission of patients within 30 Days, this is the same timeframe as that measured in the medical readmission rate. International data demonstrates a variation in 30 day readmission rates for COPD patients. A systematic review of 34 studies has found the range of avoidable readmissions can vary between 5 and 79% with a median of 27%1. A more recent review by Shah et al suggest that patients hospitalized for COPD are likely to have a 30-day re-admission rate of 22.6%2
Measurement methodology and data sources
KPI 1: Median LOS for patients admitted with COPD
KPI 2: % re-admission to same acute hospitals of patients with COPD within 30 days.
Local HIPE Data extrapolated quarterly for analysis and publication
Targets
KPI 1: Median LOS for patients admitted with COPD – 5 Days
KPI 2: % re-admission to same acute hospitals of patients with COPD within 30 days – 22.6%
Performance
KPI 1: Median LOS for patients admitted with COPD
- Beaumont Hospital do not have a MAU
- Cavan and Drogheda Hospitals are achieving the national target for KPI 1 in Q4 2023
- Beaumont and Connolly Hospitals are not achieving national target for KPI 1 in Q4 2023
- no national comparable data is available
KPI 2: % re-admission to same acute hospitals of patients with COPD within 30 days
- RCSI Hospitals achieving target for KPI 2 in Q4 2023
- Note: data outlined is re-admission within 30 Days to same acute hospital, the same timeframe as measured in the medical readmission rate. National KPI for COPD measures readmission within 90 Days.
- recent international data suggests a re-admission rate for COPD patients of 22.6% within 30 days
- no national comparable data is available
1 Van Walraven C, Bennett C, Jennings A, Austin PC, Forster AJ. Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ. 2011;183 (7):E391–E402.
2 Shah T, Press V, Huisingh-Scheetz M, White SR. COPD readmissions: addressing COPD in the era of value-based health care. Chest. 2016;150 (4):916–926.
Patients who have been identified as no longer requiring acute medical care i.e. medically fit for discharge, but remain in hospital waiting for provision of either Community Home Care Support, Long Term Care or Rehabilitation are described as experiencing a delayed transfer of care (DTOC). This delay can result in increased likelihood of hospital acquired infection or a loss of confidence and necessary skills for daily living required for returning home. As well, their ongoing inappropriate accommodation in an acute bed causes resultant delays in accommodating emergency / elective patients requiring acute hospital admissions.
Measurement methodology and data sources
- periodic local data submitted weekly to the BIU and Hospital Group:
- number of patients identified as no longer requiring acute medical care and experiencing a Delayed Transfer of Care (DTOC) to Home or Residential Care Facility (RCF)
- length of time (days) from being identified as no longer requiring acute medical care, but require either provision of a Home Care Package (HCP) to enable discharge home or Residential Care Facility (RCF) accommodation and actual discharge to either Home or Residential Care Facility
Target
- no more than 30 patients experiencing an inappropriately delayed discharge within the RCSI Hospital Group
- provision of HCP and discharge home within 5 days of being identified as no longer requiring acute medical care / accommodation
- discharge to Residential Care Facility within 7 days of being identified as no longer requiring acute medical care
Performance
RCSI Hospital Group Delayed Transfers of Care (DTOC) 2024 v 2023 – Average Monthly
- target of <30 patients achieved for reporting period (n=22 February)
- 41% decrease 2024 / 2023 YTD in the average number of patients experiencing a “DTOC”
- 57% decrease (n=29) Feb-24 v Feb-23
- monthly average of 862 bed days YTD were inappropriately utilised for accommodation of patients experiencing “DTOC” – equating to an acute bed day capacity equivalent to the monthly treatment and accommodation of 123 elective / emergency patients (based on a 7 day average length of stay)
- nationally 34% decrease 2024 / 2023 YTD in the average number of patients experiencing a “delayed discharge”. 34% decrease (n=195) Feb-24 v Feb-23
- national average of n=375 for February therefore not achieving national target of n=350.
- 57% decrease (n=29) Feb-24 v Feb-23
Delayed Transfer of Care average period (days) identified for RCF -> RCF placement
- target for successfully transferring patients from Hospitals to Residential Care Facility achieved by Beaumont and Cavan Hospitals
- no eligible patients for RCF for Navan in monthly reporting period
DTOC average period (days) identified for HCP identification -> Discharge Home
- target for successfully transferring patients home with HCP achieved by Beaumont Hospital
The role of COVID-19 testing in assisting with decision-making regarding transfers to congregated settings. People for admission to a Long Term Residential Care Facility (LTRCF) should be tested for SARS-CoV-2. This is to help identify most of those who have infection, but it will not detect all of those with infection (Guidance on COVID-19 Admissions, transfers to and discharges from residential care facilities V1.2 23.12.20).
Measurement methodology and data sources
Testing should be performed within three days of planned admission/transfer to the LTRCF.
Target
100% compliance of all residents who meet the criteria is tested and result available prior to admission/transfer
Performance – August 2022
- national data not available
- from September 2022, as per national policy V1.8 published 15.09.22, testing of asymptomatic residents on transfer or admission is generally not required
The National Patient Safety Office via the National Healthcare Quality Reporting System (NHQRS) provides retrospective data yearly on a suite of metrics across many aspects of healthcare. The metrics represented beneath cover the time period 2019-2021 and are therefore reflective of the healthcare delivery during the COVID-19 pandemic.
Rationale for measurement:
It is important that every hospital measures and monitors mortality from specific conditions. Over the past two decades in-hospital mortality patterns have been used as one key indicator of quality of care internationally. The metrics represented beneath are reflective of a number of conditions managed in acute hospital services:
- Principal diagnosis of Acute Myocardial Infarction (AMI)
- Principal diagnosis of Ischaemic Stroke
- Principal diagnosis of Haemorrhagic Stroke
Measurement methodology
The data examines age-sex standardised in-hospital mortality rates (ASR) within 30 days of admission for AMI, Ischaemic Stoke and Haemorrhagic Stroke over the time period 2019-2021. ASR allows the rate of an event in one hospital or country to be compared against the rate standardised for that event in another hospital or country, taking into account differences in age and sex.
Notes:
Hospitals with small numbers of cases tend to have unstable rates and wider confidence intervals. For this report rates are not displayed for hospitals with less than 100 cases, although the data for these hospitals have been included in the calculation of the national and group total rates. However some hospitals with more than 100 cases may still have unstable rates and caution should be exercised in interpreting rates with wide confidence intervals. The data presented above are age-sex standardised mortality rates per 100 cases. 95% confidence intervals for hospitals and hospital groups are shown. Where the 95% confidence interval for a hospital or hospital group overlaps the 95% confidence interval of the national rate (i.e. the dashed green lines), it can be concluded that the rate is not statistically significantly different from the national rate and so is within the expected range. Where the 95% confidence interval for a hospital or hospital group does not overlap the confidence interval of the national rate, it implies that the mortality rate is statistically significantly different from the national rate and is therefore outside the expected range. Any hospital with a rate that is statistically significantly higher than the national rate is marked in orange.
ACUTE MYOCARDIAL INFARCTION (ACUTE MI)
Description
AMIs are life-threatening emergencies that happen when the coronary arteries, the blood vessels supplying blood to the heart muscle, are suddenly blocked. Lack of blood supply damages the heart muscle, weakening its function or stopping it altogether.
Definition
Age-sex standardised in-hospital mortality within 30 days for acute myocardial infarction (AMI) (heart attack) is defined as the number of patients aged 45 and over who die in hospital within 30 days of being admitted with a principal diagnosis of an AMI, as a proportion of the total number of patients aged 45 and over admitted to that hospital with a principal diagnosis of an AMI.
Rationale for measurement
The number of adults with clinically diagnosed coronary heart disease is expected to rise to more than 103,000 by 2020. One of the potential consequences for those with heart disease is that they may experience an AMI which is one of the leading causes of death in Ireland.
Age-sex standardised in-hospital mortality rates within 30 days of admission for AMI by hospital group and hospital, 2019-2021 (OECD age-sex standardization, aged 45+ only)
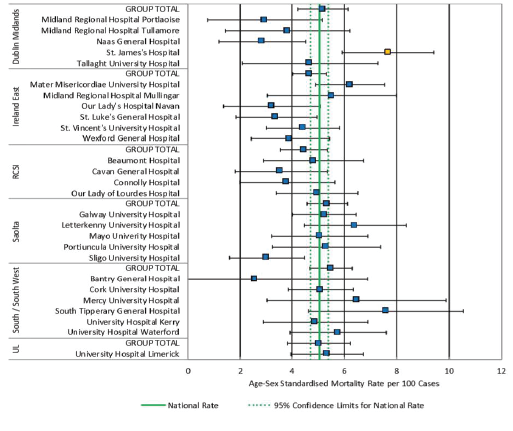
- All hospitals in the RCSI Hospital Group are within the expected range for patients admitted with a principal diagnosis of AMI.
Description
An ischaemic stroke is caused by death of brain cells in a localized area due to inadequate blood flow caused by ischaemia (blood clot). This is the most common type of stroke, accounting for approximately 85% of strokes.
Definition
The number of patients aged 45 years and over who die in hospital within 30 days of being admitted with a principal diagnosis of an ischaemic stroke, as a proportion of the total number of patients aged 45 years and over admitted to that hospital with a principal diagnosis of an ischaemic stroke.
Rationale for measurement
Stroke is a leading cause of morbidity and mortality in Ireland; over 7,000 people in Ireland are hospitalised following stroke each year and approximately 2,000 people die as a result of stroke each year. Ischaemic strokes account for approximately 85% of all strokes which result in hospitalisation in Ireland annually.
Age-sex standardised in-hospital mortality rates within 30 days of admission for ischaemic stroke by hospital group and hospital, 2019-2021 (OECD age-sex standardization, aged 45+ only)
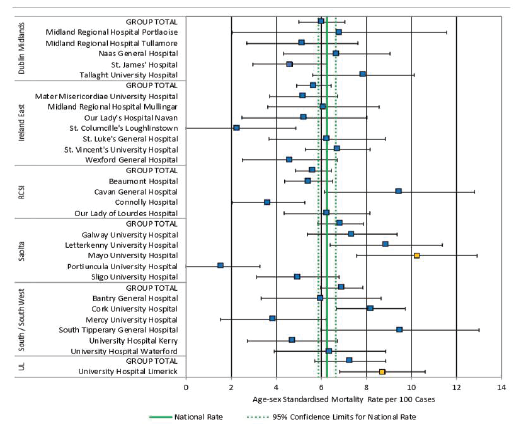
- All hospitals in the RCSI Hospital Group are within the expected range for patients admitted with a principal diagnosis of ischaemic stroke
Description
A haemorrhagic stroke is the sudden death of brain cells in a localised area due to inadequate blood flow caused by a haemorrhage (bleeding). Haemorrhagic stroke occurs when a blood vessel in the brain leaks or ruptures.
Definition
The number of patients aged 45 years and over who die in hospital within 30 days of being admitted with a principal diagnosis of haemorrhagic stroke, as a proportion of the total number of patients aged 45 years and over admitted to that hospital with a principal diagnosis of haemorrhagic stroke.
Rationale for measurement
Stroke is a leading cause of morbidity and mortality in Ireland; over 7,000 people in Ireland are hospitalised following stroke each year and approximately 2,000 people die as a result of stroke each year.
Age-sex standardised in-hospital mortality rates within 30 days of admission for haemorrhagic stroke by hospital group and hospital, 2019-2021
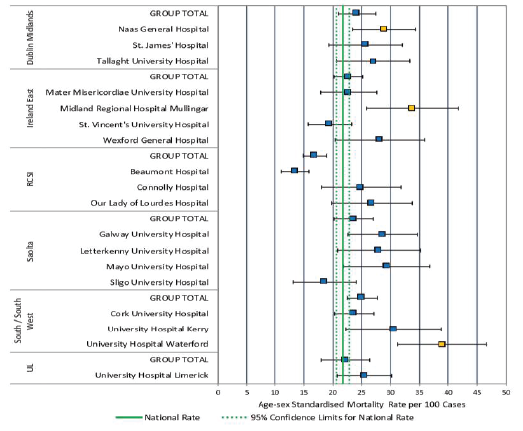
- All hospitals in the RCSI Hospital Group are within the expected range for patients admitted with a principal diagnosis of haemorrhagic stroke
- Principal diagnosis of Acute Myocardial Infarction
- Principal diagnosis of Heart failure
- Principal diagnosis of Ischaemic Stroke
- Principal diagnosis of Haemorrhagic Stroke
- Principal diagnosis of Chronic obstructive pulmonary disease
- Principal diagnosis of Pneumonia
In-hospital mortality is defined as death occurring during the hospital stay.
The National Audit of Irish Hospital Mortality (NAHM) has provided mortality data from 44 publicly funded Irish hospitals. This data relates to acute cases admitted to hospital, where the principal reason for admission, established at time of discharge is one of six key diagnoses, Acute Myocardial Infarction, Heart Failure, Ischaemic Stroke, Haemorrhagic Stroke, COPD and Pneumonia.
The purpose of the NAHM report is to provide an analysis of in-hospital mortality to patients, the public and the wider healthcare system, and to communicate the recommendations made on the basis of the findings. This report provides reassurance that there is a process in place to monitor mortality data, and any outliers are acted upon and learnings shared.
Rationale for measurement
It is important that every hospital measures and monitors mortality from specific conditions. Over the past two decades in-hospital mortality patterns have been used as one key indicator of quality of care internationally.
Measurement methodology
Standardised Mortality Ratio (SMR) is a commonly used statistical method for examining hospital mortality patterns within a country or within a group of hospitals. The SMR compares the observed number of deaths to the expected number of deaths for a specific diagnosis. The graphs in this section are used to assess performance outcomes for individual Hospitals in comparison to the national average (straight line). The dashed lines in each graph represent the 99.8% control limits. It is very unlikely a Hospital would lie outside these limits by chance. A finding of a statistical outlier does not indicate that a hospital is providing poor quality of care, but rather that there is a difference between the expected value and the result that is unlikely to have arisen from random variation alone.
Only hospitals with 100 or more admissions in each diagnosis are included for analysis by NAHM in order to ensure statistical reliability.
ACUTE MYOCARDIAL INFARCTION (ACUTE MI) – IN-HOSPITAL STANDARDISED MORTALITY RATIO OF ADMISSION FOR AMI, 2021
The medical term for a heart attack is acute myocardial infarction (AMI). A heart attack is a life-threatening medical emergency in which the supply of blood to the heart is suddenly blocked, usually by a blood clot. The lack of blood or blockage to the heart can seriously damage the heart muscles (Irish Heart Foundation, 2020). There are two types of heart attack that are diagnosed by a trace of the heart rhythm known as an electrocardiogram (ECG):
- ST-elevation myocardial infarction (STEMI)
- Non-ST-elevation myocardial infarction (NSTEMI)
For the purposes of this report, both subtypes are grouped together under the diagnosis of AMI
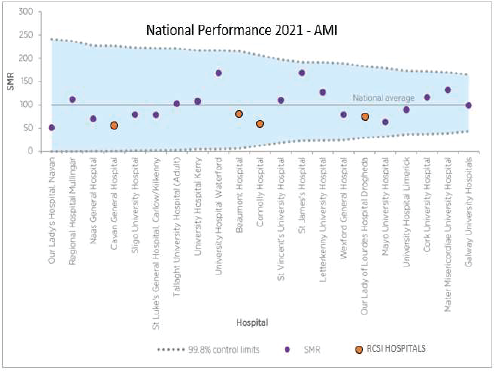
- Beaumont Hospital, Cavan Hospital, Connolly Hospital and Drogheda Hospital had a SMR within the expected range for patients admitted with a principal diagnosis of AMI
HEART FAILURE – IN-HOSPITAL STANDARDISED MORTALITY RATIO OF ADMISSION FOR HEART FAILURE, 2021
Heart failure is a medical condition where the heart does not work as efficiently as it should. This means that due to reduced blood flow, the blood is unable to deliver enough oxygen and nourishment to the body in order to allow it to work normally. This can cause various symptoms such as shortness of breath, muscle and leg swelling. Some 80% of heart failure patients suffer from physical symptoms, such as severe breathlessness and fatigue (Irish Heart Foundation, 2021).
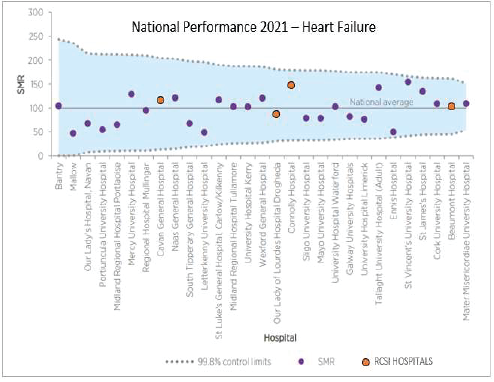
- Beaumont Hospital, Cavan Hospital, Connolly Hospital and Drogheda Hospital had a SMR within the expected range for patients admitted with a principal diagnosis of Heart Failure
ISCHAEMIC STROKE – IN-HOSPITAL STANDARDISED MORTALITY RATIO OF ADMISSION FOR ISCHAEMIC STROKE, 2021
A stroke is a serious, life-threatening medical condition. An Ischaemic stroke happens, when the blood supply to the brain is stopped due to a blood clot. Ischaemic strokes account for approximately 85% of all strokes. Like all organs, the brain needs oxygen and nutrients provided by the blood in order to function properly. If the supply of blood becomes interrupted or cut off, brain cells begin to die within minutes. When the affected brain cells die, the motor, visual or cognitive function (e.g. speech) controlled by these cells stops working. Depending on the location and size of the affected area, a stroke can lead to very significant brain injury and disability, and possibly even death.
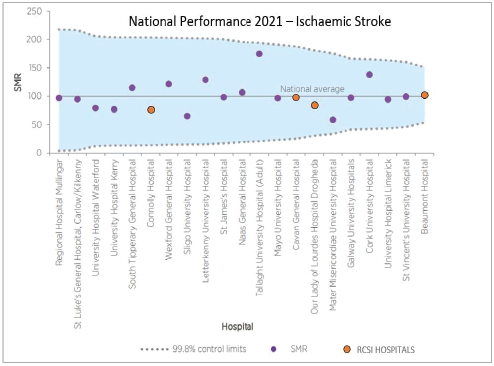
- Beaumont Hospital Cavan Hospital, Connolly Hospital and Drogheda Hospital had a SMR within the expected range for patients admitted with a principal diagnosis of Ischaemic Stroke
HAEMORRHAGIC STROKE – IN-HOSPITAL STANDARDISED MORTALITY RATIO OF ADMISSION FOR HAEMORRHAGIC STROKE, 2021
Haemorrhagic stroke occurs when a weakened blood vessel supplying blood to the brain ruptures, causing bleeding into or around the brains. Haemorrhagic strokes account for approximately 15% of strokes (King’s College London for the Stroke Alliance for Europe (SAFE), 2017).
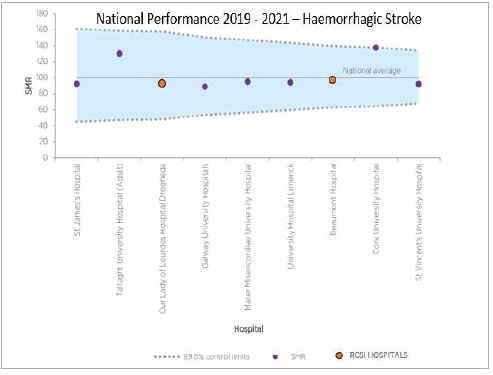
- Beaumont Hospital and Drogheda Hospital had an SMR within the expected range for patients admitted with a principal diagnosis of Haemorrhagic Stroke.
- Due to the low numbers of cases with a principal diagnosis of haemorrhagic stroke, data for the 3-year period from 2019 to 2021 were combined by NAHM. Only 9 Acute Hospitals met the inclusion criteria for 2019–2021 (Cavan and Connolly Hospitals did not meet this criteria and excluded by NAHM from this data set).
CHRONIC OBSTRUCTIVE PULMONARY DISEASE (COPD) – IN-HOSPITAL STANDARDISED MORTALITY RATIO OF ADMISSION, 2021
Chronic obstructive pulmonary disease (COPD) is a disease that causes inflammation of the lungs and obstruction of the airways which is usually progressive and only partially reversible. It may be a life-threatening condition and is one of the most common respiratory diseases in Irish adults. It usually affects people over the age of 35 years. The disease causes increasing breathlessness, a chronic cough and increasing mucous production. Severe cases can result in frequent intervention at primary care level, hospital admissions, and often premature death. It is a significant cause of morbidity and mortality in Ireland. The most common specific cause of emergency hospital admission among adults in Ireland is COPD.
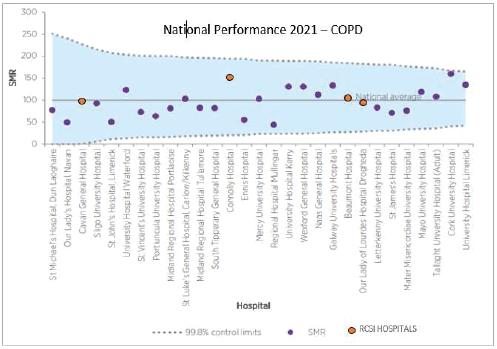
- Beaumont Hospital, Cavan General Hospital, Connolly Hospital and Drogheda Hospital had an SMR within the expected range for patients admitted with a principal diagnosis of COPD
PNEUMONIA – IN-HOSPITAL STANDARDISED MORTALITY RATIO OF ADMISSION FOR PNEUMONIA, 2021
Pneumonia is an acute inflammatory condition (swelling) of the tissue in one or both lungs. There are clusters of tiny air sacs at the end of the breathing tubes in the lungs, which will fill with air when lungs are healthy. If an individual has pneumonia, these tiny sacs become inflamed and fill up with fluid, which makes breathing painful and limits oxygen intake.
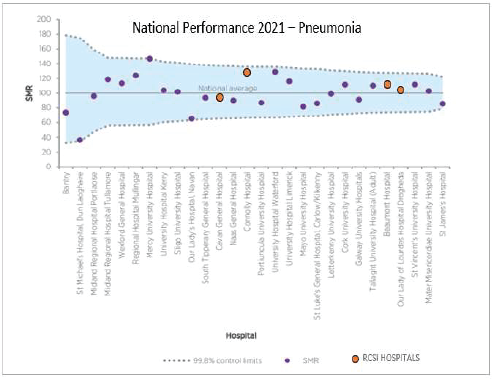
- Beaumont Hospital, Cavan General Hospital, Connolly Hospital and Drogheda Hospital had an SMR within the expected range for patients admitted with a principal diagnosis of pneumonia
Notes:
The standardised mortality ratio (SMR) is another method that adjusts for population differences. It is a measure of mortality that allows individual hospitals to compare their observed death rate against the rate that would be expected in that hospital if other variables affecting mortality could be taken into consideration. Analysis of SMRs is based on the principal diagnosis of the patient recorded in HIPE, i.e. the diagnosis that was established after investigation and found to be responsible for the episode of admitted patient care. It is important to note, however, that the principal reason for a person’s hospitalisation is not always the reason for their death.
The “expected deaths” are calculated from national data using statistical techniques to account for differences in patient factors. These factors include: age; sex; deprivation; whether patients were in receipt of palliative care treatment in hospital; number of previous admissions in the past year; source and type of admission (for example, from home or a nursing home, or an emergency transfer from another acute hospital); and the Charlson Comorbidity Index (CCI) (Charlson et al., 1987), which is a measure of comorbidity. The CCI data are derived from additional diagnoses coded on the HIPE episode.
The Irish National Intensive Care Unit Audit (INICUA) is published by NOCA. INICUA examines data from Intensive Care Units (ICU)s across Ireland & the UK. The data, which is submitted to INICUA via an ICU portal, allows hospitals to monitor and benchmark the care they provide against other centres. ICU care in the RCSI Hospital Group is provided in Beaumont Hospital, Cavan Monaghan Hospital, Connolly Hospital and Drogheda Hospital.
ICU patients are usually the sickest patients in the hospital and mortality can be high for this cohort. Therefore, several metrics are extrapolated quarterly from the ICU portal by the RCSI HG for publication & monitoring. These metrics are (1) unplanned re-admissions to ICU within 48 hours, (2) high – risk admissions from the ward (3) high – risk sepsis admissions from the ward and (4) out of hours discharges to the ward (not delayed). INICUA data from 2022 is included for comparison.
Measurement Methodology and data sources
- local hospital data extrapolated for analysis and publication
- Irish National Intensive Care Unit Audit (INICUA), data 20221
[1] Network Quality Report, RCSI Hospital Group (01/01/2022-31/12/2022), National Office of Clinical Audit
Targets
- An ICU unit’s performance is expected to lie within the 99.8% predicted range (dashed red lines) 998 times out of 1000.
- The predicted ranges are calculated based on the expected value for the unit and the number of admissions (or bed days for rates).
Definitions
The Sequential Organ Failure Assessment (SOFA) score is a scoring system that assesses the performance of several organ systems in the body (neurologic, blood, liver, kidney, and blood pressure/hemodynamics) and assigns a score based on the data obtained in each category. A higher SOFA score, predicts higher patient mortality.
1. Unplanned readmission to an Intensive Care Unit within 48 hours
Rationale for measurement
Unplanned readmission to an intensive care unit within 48 hours is an important indicator to assess quality of care in ICU. Patients with an unplanned readmission to ICU have a higher mortality rate and readmission is associated with a longer stay in hospital.
Numerator: Number of patients discharged from ICU who were subsequently readmitted (unplanned) to the same critical care unit within 48 hours of discharge.
Denominator: Number of ICU patients discharged to a ward within the same hospital.
Performance
- in Q4-23 Beaumont General ICU, Beaumont Neuro ICU, Cavan and Drogheda Hospitals are within the 99.8% predicted range outlined in the INICUA report 2022
- in Q4-23 Connolly Hospital is outside the 99.8% predicted range outlined in the INICUA report 2022
2. High Risk Admissions from the ward
Rationale for measurement
If patients have four or more organ dysfunctions (which means a high SOFA Score) within 24 hours of admission to ICU, it is possible that their ICU admission may have been delayed.
Numerator: The number of admissions with four or more organ dysfunctions (SOFA ≥ 2 per organ) during the first 24 hours following admission.
Denominator: The number of admissions from a ward (or intermediate care or obstetric area) in the same hospital.
Performance
- in Q4-23 all hospital sites are within the 99.8% predicted range outlined in the INICUA report 2022
- Cavan Hospital Q4 23 data is not available at the time of report publication
3. High Risk Sepsis Admissions from the ward
Rationale for measurement
Sepsis is a very important condition in critically ill patients and can be difficult to diagnose in the early stages. Failure of four or more organ systems in this cohort of patients (which means a high SOFA Score), occurring within 24 hours of ICU admission suggests that ICU admission may have been delayed.
Numerator: The number of admissions with infection who have four or more organ dysfunctions (SOFA ≥ 2 per organ) during the first 24 hours following admission.
Denominator: The number of admissions from a ward (or intermediate care or obstetric area) in the same hospital.
Performance
- in Q4-23 all hospital sites are within the 99.8% predicted range outlined in the INICUA report 2022
- Cavan Hospital Q4 23 data is not available at the time of report publication
4. Out of Hours Discharges to the ward (not delayed)
Rationale for measurement
Out-of-hours discharge from an ICU (between 22.00 hours and 06.59 hours) can be associated with both in-hospital death and ICU readmission.
Numerator: The number of admissions discharged from the critical care unit between 22.00 and 06.59 and not delayed (i.e. not declared ready for discharge by 18.00 on that day)
Denominator: The number of patients discharged to a ward in the same hospital.
Performance
- in Q4-23, all hospital sites are within the 99.8% predicted range outlined in the INICUA report 2022
- Cavan Hospital Q4 23 data is not available at the time of report publication
The Irish National Audit of Stroke (INAS) provides an annual report in conjunction with the National Office of Clinical Audit (NOCA). The aim of collecting and publishing this data is to assist in monitoring and improving stroke services. It also allows individual units to benchmark their performance against other units in Ireland.
Rationale for measurement
Door to Imaging (DTI): this is a term used to indicate the time interval between the arrival of the patient at the hospital and the time of the first brain scan. The acute management for ischaemic and haemorrhagic strokes differs substantially. Timely performance of a brain scan is the only reliable method of distinguishing between an ischemic and haemorrhagic cause.
Door to needle (DTN): this is a term used to indicate the time interval between the arrival of the patient at the hospital and the time of thrombolysis treatment (using medication to breakdown blood clots which have formed in blood vessels) where clinically indicated. Thrombolysis can be of benefit to patients with acute ischaemic stroke, not all patients who receive imaging will meet the criteria for thrombolysis. The window of opportunity for effective thrombolysis is four and a half hours from the onset of the stroke.
Measurement Methodology and data sources
Targets
- Door to imaging: < 60 minutes of arrival at hospital (Royal College of Physicians, 2016)
- Door to needle time < 60 minutes (Irish Heart Foundation, 2015)
Performance
Door to Imaging (DTI)
- Beaumont Hospital is achieving target of 60 minutes in December 2023 (n=35 cases)
- Cavan Hospital is not achieving target of 60 minutes in December 2023 (n=12 cases)
- Connolly Hospital is not achieving the target of 60 minutes in December 2023 (n=11 cases)
- Drogheda Hospital is achieving the target of 60 minutes in December 2023 (n=29 cases)
Door to needle (DTN)
- Beaumont Hospital is achieving target of 60 minutes in December 2023 (n=4 cases)
- Thrombolysis can be of benefit to patients with acute ischaemic stroke. Not all patients who receive imaging will meet the criteria for thrombolysis
- Cavan Hospital is achieving target of 60 minutes in December 2023 (n=2 cases)
- Thrombolysis can be of benefit to patients with acute ischaemic stroke. Not all patients who receive imaging will meet the criteria for thrombolysis
- Connolly Hospital is achieving target of 60 minutes in December 2023 (n=1 case)
- Thrombolysis can be of benefit to patients with acute ischaemic stroke. Not all patients who receive imaging will meet the criteria for thrombolysis
- Drogheda Hospital is achieving target of 60 minutes in December 2023 (n=3 cases)
- Drogheda Hospital had no eligible cases in September and November 2023
- Thrombolysis can be of benefit to patients with acute ischaemic stroke. Not all patients who receive imaging will meet the criteria for thrombolysis
A stroke occurs when the blood supply to the brain is interrupted or reduced. This deprives the brain of oxygen and nutrients, which can cause the brain cells to die. A stroke may be caused by a blocked artery (ischaemic stroke) or the leaking or bursting of a blood vessel (haemorrhagic stroke). Thrombolysis is a treatment to dissolve clots in blood vessels, improve blood flow, and thus help prevent damage to tissues and organs. Thrombolysis can be of benefit in patients with acute ischaemic stroke. The window of opportunity for effective thrombolysis is four and a half hours from the onset of the stroke. Therefore within that timeframe, a firm diagnosis of ischaemic stroke must be made.
Measurement methodology and data sources:
Periodic local data extracts extrapolated for analysis and publication
Rationale for measurement
Stroke is known to be a leading cause of disability and death in patients worldwide. Care in a Stroke Unit is provided in hospital by nurses, doctors and therapists who specialise in looking after stroke patients and work as a co-ordinated team. Evidence shows, that patients who receive this type of care are more likely to survive their stroke, return home and become independent in caring for themselves. Hospital based Stroke Units are associated with a reduction in death and institutional care of around 20%, with one additional patient returned to community living for every 20 patients treated (Stroke Clinical Care Programme, 2012).
Measurement methodology and data sources
KPI1 % of acute stroke patients who spend all or some of their hospital stay in an acute or combined stroke unit*
KPI2 for acute stroke patients admitted to an acute or combined stroke unit, the % of their hospital stay spent in the stroke unit*
KPI3 % of patients with confirmed acute ischaemic stroke who receive thrombolysis
KPI6 % of cases have a swallow screen completed
The data is recorded at hospital level via a Stroke Portal within the HIPE file and data is collected by clinical staff. The data is reported quarterly to the BIU via the Health Pricing Office and the National Stroke Programme.
*A Stroke Unit is defined by the European Stroke Organisation as: “a geographically discreet area with the capacity to monitor and regulate basic physiological function, access to immediate imaging and is staffed by a specialist multidisciplinary team”.
Targets
KPI1 90% of acute stroke patients are admitted to an acute or combined stroke unit
KPI2 90% of hospital stay for acute stroke patients should be spent in an acute or combined stroke unit
KPI3 12% of patients with confirmed acute ischaemic stroke receive thrombolysis
KPI6 100% of cases have a swallow screen completed
Performance
2023 Q4 is reported.
- Cavan and Beaumont Hospitals are achieving target of 90%
- Connolly and Drogheda Hospitals are not achieving target of 90%
- KPI 1 data includes Stroke/ICU/CCU/HDU beds as applicable
- Connolly, Cavan and Beaumont Hospitals are not achieving target of 90%
- Drogheda Hospital is achieving target of 90%
- KPI 2 data includes Stroke/ICU/CCU/HDU beds as applicable
- Connolly, Beaumont, Drogheda and Cavan Hospitals are not achieving target of 12%
- KPI 3 data includes Stroke/ICU/CCU/HDU beds as applicable
- Beaumont, Drogheda and Cavan Hospitals are not achieving target of 100%
- Connolly Hospital is achieving target of 100%
Deep vein thrombosis (DVT, the formation of a blood clot in a deep vein) and pulmonary embolism (PE, a blood clot that travels to the lungs), known together as venous thromboembolism (VTE), comprise the most common preventable cause of hospital-related death. There are 5,000 cases of VTE in Ireland each year. Recent international data suggests that over 50 per cent of all VTE events are hospital acquired (defined as a VTE event occurring during hospital admission or within 30 days of discharge).
There are certain groups of hospital patients that are at increased risk of VTE, including maternity patients, patients with cancer, having surgery, patients who have had with major trauma or patients who have been immobilised. There is strong evidence that (1) by taking specific steps to identify high-risk hospital patients (risk assessment) and (2) by implementing VTE prevention measures where appropriate, up to 70% of these VTE events can be prevented thus saving lives.
Currently robust data relating to patterns of VTE incidence within the Republic of Ireland is lacking. A recent study(1) from Ireland East Hospital Group suggested an incidence of 1.44 (95% CI 1.36 to 1.51) per 1000 per annum. A 2018 National Medication Safety Improvement Programme HSE (Quality Improvement Division) report(2) cited an incidence of 8 per 1000 discharges (rate 0.8). UK incidence rates have been reported as 1–2 per 1,000.
Rationale for measurement
It is estimated that 70% of healthcare-associated VTE is potentially preventable with appropriate VTE prophylaxis. A VTE risk assessment performed on admission and at 24 hours (at a minimum) identifies which risks are present and clarifies whether the overall risk is high enough that the patient needs VTE prophylaxis.
Measurement methodology and data sources:
- local HIPE Coding Data extrapolated quarterly from NQAIS Clinical for analysis and publication
Rate of Hospital Acquired VTE per 1,000 (In-Patient Discharges) – Q4 2023
- Numerator: Number of adult (16+) inpatient discharges with a length of stay greater than 2 days with HIPE flagged hospital acquired diagnosis of VTE per quarter
- Denominator: Number of adult (16+) inpatient discharges with a length of stay of 2 or more days per quarter
- The number of readmissions with hospital acquired VTE within 30 days is also reflected
Performance
- Beaumont & Connolly Hospitals’ performance is above the rate of 0.8 for Q4-23
- Cavan/Monaghan and Drogheda Hospitals’ performance is below the rate of 0.8 for Q4-23
- No national comparable data is available, RCSI HG data presents only those cases which have been confirmed as Hospital Acquired VTE
References:
1. Hospital-acquired venous thromboembolism: Barry Kevane, Mary Day, Noirin Bannon, Leo Lawler, Tomas Breslin, Claire Andrews, Howard Johnson, Michael Fitzpatrick, Karen Murphy, Olivia Mason, Annemarie O’Neill, Fionnuala Donohue, Fionnuala Ní Áinle. BMJ Open Jun 2019, 9 (6) e030059; DOI: 10.1136/bmjopen-2019-03005
2. Preventing blood clots in Hospitals. Improvement Collaborative Report National Recommendations and Improvement Toolkit. July 2018. National Medication Safety Improvement Programme HSE Quality Improvement Division

